What is Transcranial Magnetic Stimulation?
Transcranial magnetic stimulation (TMS) is a treatment used to treat severe, treatment-resistant depression, anxious depression, and more recently obsessive compulsive disorder (OCD). It is a unique treatment, because it is not medication. It is a very targeted treatment that uses MRI-strength magnetic pulses which treat the specific neural networks related to the mental illness we are trying to help.
How does TMS work?
Instead of medications that inevitably flow throughout the body, TMS focuses on a specific target area which is why the treatment has very few side effects. For example, for major depressive disorder, TMS focuses on an area called the dorsolateral prefrontal cortex (DLPFC). When the magnetic waves from TMS enter the brain, they transform into electrical waves and start activating this area (the DLPFC) that has been less active since the depression began. Researchers believe depression may be a result of disrupted brain networks that aren’t working the way they should. Targeting the DLPFC helps heal that deep brain network to get it working as it should. Day-by-day, the neural connections are repaired, and your depression will usually improve after four weeks of treatment. We like to call it “training the brain to be happy again!”
The pulses do not hurt, though it’s possible they could feel uncomfortable at first. Most patients feel little to no discomfort after the first few sessions. It is not anything like electric convulsive therapy (ECT). Patients are alert and awake throughout treatment on a comfortable cushioned chair (sometimes so comfortable, our patients start to fall asleep!). Usually they watch tv, read a book, or listen to music to pass the time. And afterwards, they are able to drive, lift heavy machinery. Whatever they’d normally do in their day.
What does a TMS session look like?
The protocols for TMS are currently approved for 36 sessions (five days/week). Each session lasts around 25 minutes from the time the patient arrives to when they are done. Intermittent theta burst stimulation (iTBS) is an equivalent option that performs the same treatment even faster (under five minutes). It’s a great option if time is a concern (you can read more about iTBS here). For the actual treatment, the TMS Coordinator will place the treatment coil in the exact right position over the DLPFC and start treatment. During treatment, you can chat with your TMS Coordinator, watch tv, read a book, or listen to music. You will be completely awake and alert the whole time.
Does TMS only treat depression?
There are several variations of TMS that are currently being used to treat patients and others still being tested, including: iTBS, Stanford Neuromodulation Treatment (SNT or SAINT), and OCD treatment just to name a few. This is an exciting field within psychiatry that may be able to treat diverse forms of mental illness including: PTSD, alcohol and substance use disorder, schizophrenia, and more.
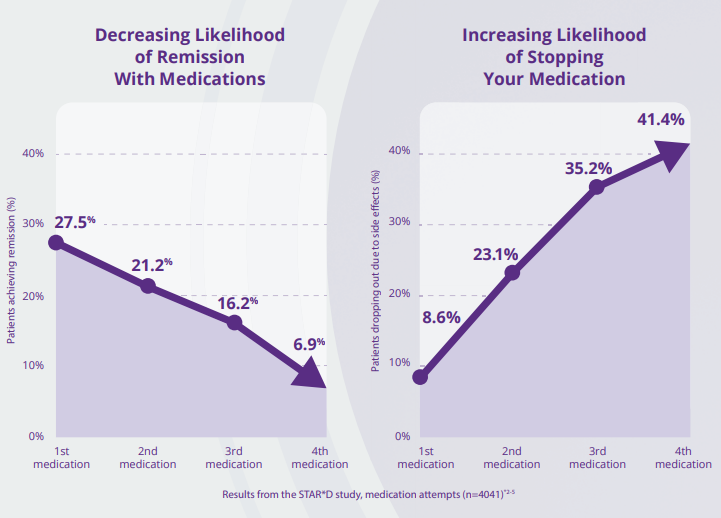
The treatment is incredibly effective at treating depression even in patients where previous medications have not worked. In fact, research shows that TMS is greater than 3 times more effective than medication once a patient has failed three or more medication trials. We’ve personally seen many patients who thought there was nothing else that could treat their depression who went into complete remission following TMS treatment.
How to get started with TMS treatment?
To learn more about TMS, ask any questions, or find out how to get started with treatment please contact us at (212) 707-8662 or email us at [email protected]!
TMS is covered by most major insurance companies, and our office also offers CareCredit to make sure money is not a barrier to getting the treatment you need.
